
General information and symptomatology
The blood vascular system handles the return of blood after it has carried oxygen and nutrients to the tissues via. This system, with walls which at the source are composed of both elastic and muscle tissue, is also equipped with valves that support effective flow-return. The normal direction of vascular circulation is from the peripheral regions (feet and hands) towards the heart. 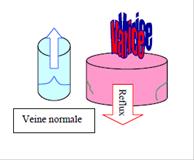
Venous insufficiency is linked to abnormal relaxation of the vascular walls, causing dilation and stretching of the walls and gaps that allow blood to pool in the feet as a result.
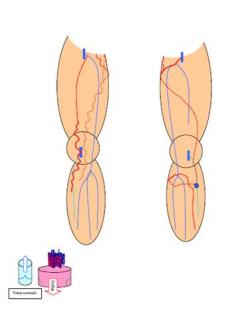
Varicose veins are therefore veins that have become more dilated and longer. Thus they take a circuitous route that is totally or partially visible under the skin. This is a very common condition, mostly linked to heredity, pregnancy, obesity, prolonged periods of standing as well as lack of regular physical activity, chronic exposure to intense heat and chronic use of high-heeled shoes. It is initially benign, but sometimes develops into a serious crippling illness.

The most commons symptoms are heaviness, pain, rupturing of the varicose veins resulting in external bleeding, as well as varicose eczema, dermatitis (inflammation of the skin) and ulcers.
Blood stagnating in the veins and irritant catabolites (waste) contained in blood, also promote the onset of phlebitis (inflammation of the veins possibly accompanied by blood clots) usually with no notable features when superficial. Sometimes it extends to the deep vein network and would then require more serious medical treatment over several months, exposing the patient to the risk of pulmonary embolism due to migration of a blood clot fragment.
Unsightly imperfections are also to be taken into account and are sometimes the primary reason for a consultation.
Assessment
A detailed assessment is required in order to recommend the treatment approach most appropriate for the stage of venous insufficiency presented by each patient, in order to guarantee functional, aesthetic, sustainable results.
An accurate assessment by means of a clinical examination combined with an exploratory ultrasound during consultation makes it possible to perform individual vascular mapping for each patient: normal veins are shown in blue and diseased veins to be treated, in red.
Once this has been done, the proposed treatment approach will itself be individualised.
Treatments
When indicated, compression, sclerosis and echosclerosis foam are recommended during consultation.
When indicated, varicose vein stripping by endovascular route or by open surgery is performed and then relayed if necessary through the sclerotic tissue to provide optimal management for each patient. If you wish, all of the surgical procedures can be performed on a day-admission basis (without spending the night at the clinic). In every case, the two factors that concern us are surgery producing aesthetically pleasing post-operative outcomes and a result that is as sustainable as possible over the long term.
In some special cases, women may present with varicose veins, pain, gynaecological heaviness or pain located in the lower abdominal region due to deep venous reflux in the abdomen via the veins of the small pelvis. These conditions will be treated by embolisation before any surgery is performed.
1. Compression :
Elastic band compression or stocking compression compensates for venous dysfunction by promoting blood flow return by compression of the veins, which are also better emptied by muscle exertion.


2. Sclerosis :
Sclerosis gets rid of small varicose veins by injecting these veins with a powerful product that destroys the vein wall and stimulates its regression. If the varicose vein is more prominent, the foam version of the product, which is stronger, can be used. If the varicose vein is not visible for aspiration to be performed, the procedure is carried out under ultrasound guidance (figure at right). 

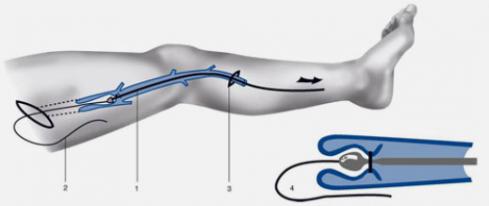
3. Varicose vein stripping :
Stripping by surgical route involves removing varicose veins after ligating them at their junctures in the deep vein – most often at the top of the thigh or the crook of the knee. This technique can be used in cases where the endovenous route is not applicable. We use the eversion technique which produces fewer post-surgical haematomata and smaller incisions which fade away over time.
Staged resections involves retracting the collateral arteries (branches) of the varicose veins by micro-incisions (2 to 3 mm) usually closed without stitches using an adhesive (steristrips). The varicose vein is extracted with a small hook. This is a complementary technique generally used in the stripping of the large saphenous veins described previously, but it can also be applied to isolated varicose branches. The small incisions also become invisible over time.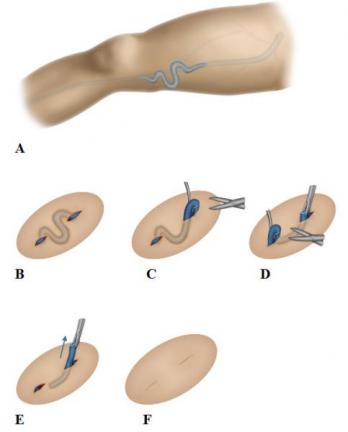

These last three techniques are routinely performed, depending on their importance, under locoregional (spinal), general or local anaesthesia.
Full mobility while keeping the area under elastic compression is authorised as soon as the anaesthetic wears off. The patient must therefore resume walking on the very day of the procedure and will normally see his surgeon in ten to fourteen days.
4. Pelvic vein embolisation :
Pelvic vein embolisation may be recommended prior to any surgical procedure if venous insufficiency is localised in the lower abdominal region (ovarian and pelvic veins) which produce symptoms in the perineum and extending into the lower limbs. Although there are exception, this problem is generally encountered after multiple pregnancies. The diagnosis is confirmed by venous phlebography. The treatment can therefore be performed at the same time: it consists in occlusion of the diseased vein with flexible metal coils and an appropriate synthetic adhesive. This entire procedure can be performed as a one-day in-patient operation (without spending the night at the clinic).
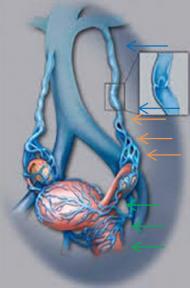
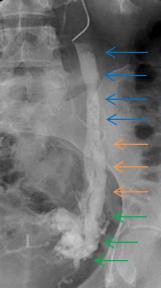

Example of right ovarian vein reflux entering the small pelvis and lateral sides of the uterus extending to the labia majora (right photo).
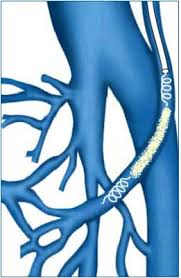


Coil embolisation : exclusion

Vein reflux towards the lower abdominal region -> two very dilated ovarian and pelvic veins
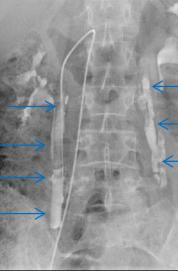

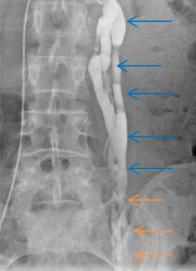
Veins filled with synthetic adhesive mixed with contrast agent: treated reflux

