
General information and symptoms
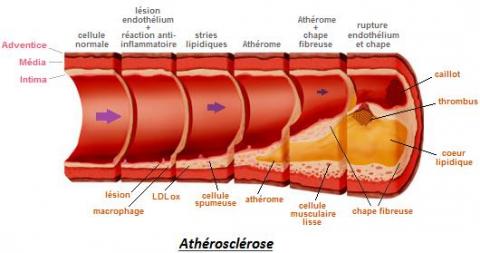
Arteries are natural conduits, like small pipes, that convey blood from the heart to the muscles and organs to feed them. These vessels can sometimes become diseased and blocked (= thrombotic): the muscles and organs depending on them suffer as a result. The most frequent cause of obstruction is atheromatosis and arteriosclerosis. Cells and harmful substances (cholesterol, etc.) are deposited in the arterial wall and this causes a reduction in vascular diameter: partial obstruction (like an hourglass or a baffle) is referred to as stenosis while total obstruction (like a plug) is referred to as thrombosis.
The following predispose to arteriosclerosis:
- Smoking
- Diabetes
- Cholesterol
- High blood pressure
- Hereditary determinants
- Significant metabolic disorders (haemodialysis, etc.)
Certain more uncommon diseases, which we also take into account, can cause arterial damage.
The symptoms experienced depend on the area affected. For example, if an artery in the right thigh is thrombotic, this will produce pain in the leg and right calf since perfusion to that area will be inadequate. The patient will no longer be able to walk for long periods without stopping to allow the pain caused by poor muscle irrigation to subside. In the most serious cases, pain can be experienced even when at rest. In extreme cases, the tissues are so deprived of blood that they die, resulting in what is known as gangrene. Such phenomena may occur (less frequently) in the organs and will thus produce pain (e.g. abdominal pain in the diseased intestinal arteries), or malfunction of the affected organ (e.g. loss of renal function, etc.).
Assessment
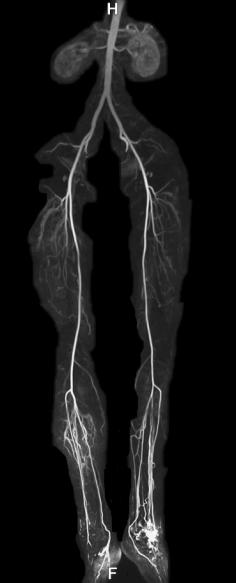
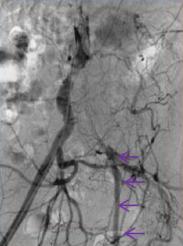
When such problems are suspected, it is helpful to come in for a consultation. Screening for diagnosis of this damage will be done by Doppler ultrasound, performed immediately during the consultation (figure 2). If suspected arterial disease is confirmed, the diagnosis will be more accurately documented by CT-scan (figures 3) or by arteriography (figure 4) or, in cases of allergic reaction to the contrast agent, by nuclear magnetic resonance or MRI (figure 5). In cases of renal insufficiency, we also have the option of performing CO2 arteriography which is harmless to the kidneys.
Figure 2
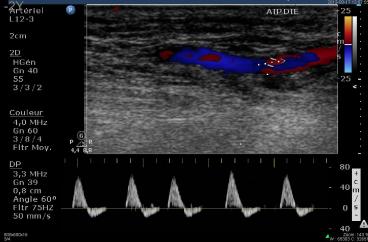
Figure 3

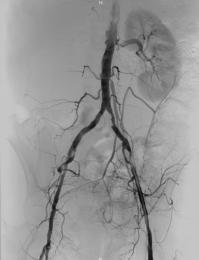

Figure 4 Figure 5

Treatment
Once the problem and your overall state of health have been evaluated (blood test, cardiopulmonary examination), we will discuss the treatment options with you.
- Irrespective of the treatment considered, medical treatment is prescribed to stabilise all of the risk factors taken down in the general information.
- In some cases, medical treatment is recommended. This will include medication to facilitate the blood circulation still existing despite the damage (anti-platelet drugs, haemorheologic drugs, and in rare cases anticoagulants).
- If necessary, treatment by endovascular route is recommended. This has the advantage of being a scar-free treatment and generally is decidedly gentler on the body than conventional surgery. This is why it is the preferred form of intervention, wherever possible, if surgery is required. This is an important feature of our approach and all the related state-of-the-art technologies are well managed and applied at Clinic Saint-Jean. They will no doubt be employed by the surgeon himself and he will follow your progress over the long term. Sometimes when arteries have not long previously been thrombotic, we can use fibrinolysis to literally melt the blood clot with special products (urokinase), always including only one puncture site (ref. to clinical case study n°3).
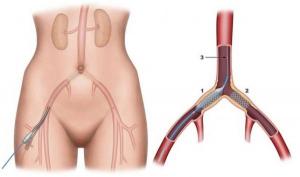
Incision-less puncture approach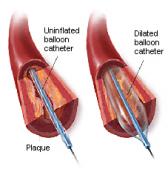

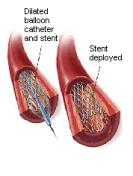
Simple balloon dilation --> In the case of an unsatisfactory result --> Stent implantation
Examples of clinical cases :
Case 1. Marked claudication (inability to walk farther than 200 metres) in a 55-year-old patient

Left iliac thrombosis and right iliac stenosis (delayed opacification at left) --> Recanalisation and stenting.
Case 2. Gangrene in the right toes and pain in the right foot preventing sleep in a 72-year-old patient too infirm to withstand general anaesthesia.


Thrombosis in 3 arteries of the calf --> Recanalisation under local anaesthesia with healing of gangrene and disappearance of foot pain.
Case 3. A female patient who had already had iliac stents fitted, presents with violent pain in the lower limbs when inactive for several hours, more intense on the left side, making walking impossible.


Thrombosis in the two previously stented iliac arteries viewed via arteriography.

Fibrinolysis performed by ordinary puncture which eliminates the entire blood clot and shows the cul-de-sac irregularities responsible for the thrombosis. Decision taken to fit covered stents:


Covered stent Covered stent in the diseased vessel
NB: Special uses for covered stents: perforated aneurysms, dissections, in-stent restenosis, etc.

After fitting of the covered stents

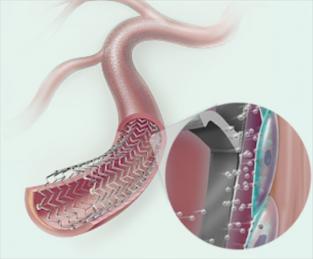
--> Other technological advances: balloons and stents filled with special drugs to reduce recurrence of the disease, etc.
--> Each innovation is evaluated and monitored …
--> In some instances, endovascular techniques are not appropriate or are impracticable. A conventional surgical solution will be proposed to you in this case. This will be an endarterectomy or a bypass.
1. Endarterectomy: this involves emptying the artery of its diseased contents in order to restore its original permeability. This type of operation is most often carried out on the femoral artery at the fold of the groin.
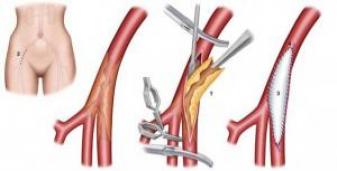
Closure can be done by ordinary suturing or, as shown here, with a small expansion piece.
2. Bypass: We use a synthetic conduit or a vein taken from the patient himself to short-circuit the thrombotic area. ---->
----> 
Post-surgical period
Endovascular techniques normally require a maximum stay of one night at the Clinic. Conventional surgical operations require a stay that varies depending on the procedure performed and the condition of the patient.
The patient can then return home or go into rehabilitation if the circumstances require this (special cases).
After the operation, the patient will receive long-term follow-up since, unfortunately, this type of disease is a life-long one and can recur at the treated site or at other locations.
