General information
Some patients require either temporary or constant dialysis. Our department offers initial dialysis and correction for haemodialysis vascular access. Our areas of competence in this discipline ranges from installation of the most basic dialysis catheter (Hickman catheter or peritoneal dialysis catheter) through a simple arteriovenous fistula in the wrist or crook of the elbow, to more extensive or complex procedures as required.
Naturally, we manage the complications linked to these access routes. There is a constant need to draw on these techniques the Saint-Jean location, and this is done with the collaboration of our colleagues in Nephrology with whom we constantly liaise.
Peritoneal dialysis catheter
Whenever possible, the patient can have a catheter fitted to his abdomen for the purpose of daily dialysis sessions at home.
The inside of the abdomen is lined with a membrane called the “peritoneum”. This membrane is richly vascularised and is permeable enough to allow toxins from the blood to be evacuated in a fluid injected via the peritoneal dialysis catheter.

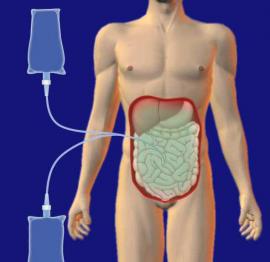
Injection of fluid into the abdomen Injection of fluid loaded with toxins
Catheter installation can be done under local anaesthesia and sedation (“temporary disconnection” without artificial respiration) or, depending on the patient, under general anaesthesia.
The length of hospitalisation is several days at most, except in special cases.
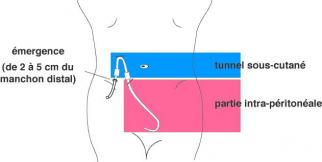
The catheter is inserted through the abdominal wall over a distance of a few centimetres to avoid spreading infection from the exterior to the interior of the abdomen.
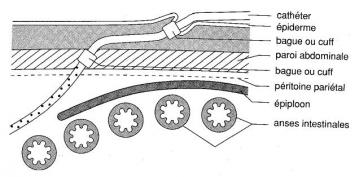
An inspection x-ray will be taken during and after the operation to check for correct positioning.

Until the wounds heal, it will be necessary to apply dressings at home.


At that time, follow-up of the patient will be the responsibility of the nephrologists.
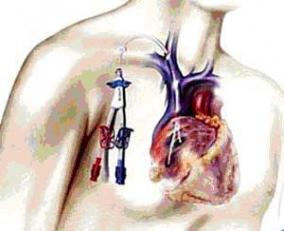
Percutaneous dialysis catheter
In some special cases, the patient will be given dialysis via a catheter originating under the clavicle, and following a path under the skin as far as a large venous trunk where the blood flow is sufficient for dialysis to be carried out correctly. The purpose of the lengthy subcutaneous path is to avoid the spread of infection from the exterior to the blood in the veins.
These catheters are fitted in patients who do not yet have a fistula and have to undergo immediate dialysis or patients who cannot or can no longer have a fistula and for whom peritoneal dialysis is contraindicated. Except for these scenarios, a fistula is to be preferred for dialysis. These catheters are made with an outlet for aspirating the blood and an inlet for reinjecting this same blood, now purified, into the dialysis machine.

The patient is then redirected to our colleagues in Nephrology who referred him.
Arteriovenous fistulas
General information
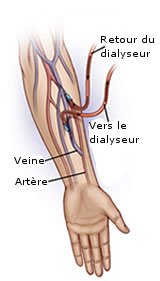
For dialysis, in order to be able to filter the patient’s blood, access is required to a blood vessel that is easy to puncture and therefore superficial and this vessel must channel a sufficient enough flow to be able to filter the patient’s blood in a reasonable time.
In humans, veins are easy to puncture as they are superficial; however, they do not provide adequate blood flow. Arteries, which have adequate blood flow, are not easy to puncture, and puncturing an artery three times a week at two sites, as is done during dialyses, would rapidly lead to thrombosis of this artery, putting the limb at risk. Veins, for their part, can be punctured more often and the risk of venous thrombosis in the arm is virtually non-existent.
The solution to this problem is to connect a vein to an artery: arterial blood flow is achieved without damage to the artery as a result of puncturing and there is the advantage of superficially-occurring veins and their safety from thrombosis. When there are no complications, these fistulas do not in any way jeopardise the function of the limb.
Native fistulas
Fistulas referred to as “native” are a communication link between the artery and the vein without the medium of a prosthesis. The section punctured during dialysis will be a natural blood vessel, i.e. the vein itself. These native fistulas are the ones with the most advantages (durability, resistance to infection, less “theft” of blood from the limb by the fistula, etc.).
The most useful type of fistula, if the patient has the appropriate blood vessels for creating it, is the wrist fistula. If the blood vessels in the forearm are not of a good quality, the fistula can be applied in the crook of the elbow.
Installing a fistula is quite easy except when the blood vessels are small. This is done in half an hour to one hour and can be done under local anaesthesia of the work area only or of the entire arm, with sedation (“temporary disconnection” without artificial respiration). Depending on the patient, general anaesthesia can sometimes be administered. Failing complications, this procedure does not require lengthy hospitalisation and can even be performed at the day hospital.
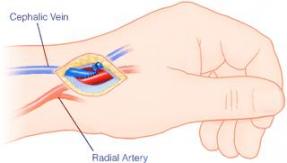
Fistula on the wrist Fistula in the crook of the elbow
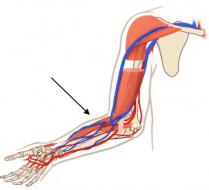
Prosthetic fistulas
 If the patient does not have an adequate enough vein in the upper limbs, the instrument used in place of the vein will be a sterile Gore-tex prosthesis, which will be placed under the skin between an artery and a deep vein.
If the patient does not have an adequate enough vein in the upper limbs, the instrument used in place of the vein will be a sterile Gore-tex prosthesis, which will be placed under the skin between an artery and a deep vein.
Doing this requires anaesthesia of the entire arm and sedation (“temporary disconnection” without artificial respiration) or more commonly, general anaesthesia.
Failing complications, this procedure does not require lengthy hospitalisation (2-3 days).
This type of fistula is a second-best to native veins which produce longer-lasting fistulas, resulting in fewer complications.


Maintenance of fistula function and complex fistulas
Fistulas can, unfortunately, change over time and lose their quality as dialysis mechanisms. In that case, they need “repair”.
Various procedures can be suggested for restoring these fistulas and returning them to their former condition. These procedures can be performed by open surgery (with scarring) as quickly as possible. We try to avoid being invasive (no scarring) by dilating the damaged areas using a balloon. If the balloon is not adequate, a stent can be put in place to keep the blood vessel resistant to dilation. If the event of recurring damage with the stent in place, a stent lined with a prosthesis (covered stent) can be put in place. There are other technical options available (coated balloon, cutting balloon, etc.) and are constantly being developed.
We are completely proficient in all of the techniques, from the more conventional ones to the more recent ones, and this enables us to optimally maintain haemodialysis vascular access over time. These techniques will without a doubt be performed by an experienced surgeon.
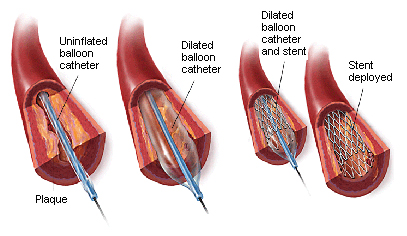
Simple balloon dilatation Fitting of a stent

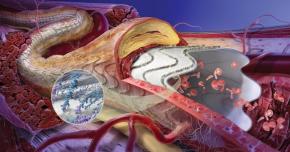
Covered stent Covered stent in a diseased blood vessel
Whenever fistulas regularly develop into thrombosis, very complex assemblies may have to be considered since the ultimate goal is obtaining a good fistula that provides high-quality dialysis that in itself enhances the patient’s quality of life.
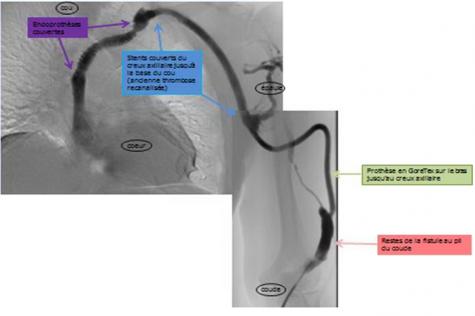
Given here is the example of a patient receiving dialysis for 17 years with the option of a graft, and no possibility for access to the upper arm or intra-abdominally. The assembly illustrated below, created in our department in several stages, currently enables the fistula to remain permanently attached to the upper left arm.