
General information and symptomatology
The carotid artery, located in the neck, is the main irrigation channel to the brain (Figures 1 and 2). It can also be the site of damage: stenosis (partial obstruction), thrombosis (complete obstruction), aneurysm in rare cases (segment dilation of the vessel) and in very rare cases, tumours.
By far the most common damage is stenosis and thrombosis. These are mainly atheromatous, i.e. composed of cell deposits and cholesterol, which attach to the carotid wall, thereby causing a reduction in the arterial lumen. These partial or total obstructions may not be manifest or may, by causing a loss of perfusion in some areas of the brain, lead to what is known as a cerebrovascular accident (stroke). This will then be manifested by paralysis, defective speech, vision, balance, awareness, etc.
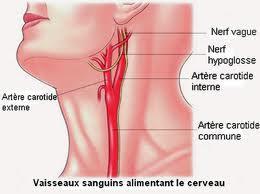
Figure 1 Figure 2
Assessment
Diagnostic screening for this type of damage is performed by ultrasound (Figure 3), and will be more accurately documented by Angioscan (Figure 4), by arteriography (Figure 5) or, in cases of allergic reaction to the contrast agent, by nuclear magnetic resonance or MRI (Figure 6).
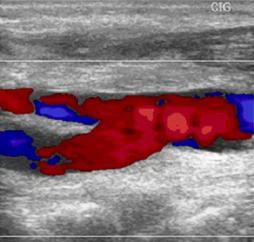

Figure 3 Figure 4

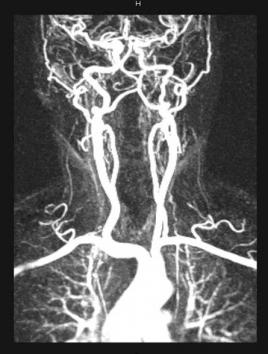
Figure 5 Figure 6
Treatment
When deemed necessary (the indications are evaluated on a case-by-case basis), in order to prevent a stroke in the first instance or a more severe recurrence of a previous stroke, our centre can recommend the most appropriate surgery which will of course be performed by a trained physician.
At present, when surgical management is indicated, it may take the form of conventional surgery (incision) or endovascular route (incision-less puncture of the artery).
In the case of conventional surgery, the carotid artery is approached by an oblique incision in the neck which will over time blend in with the skin folds. The artery is emptied of its abnormal contents (Figures 7) and closed by ordinary suturing (Figure 8) or, if the blood vessel diameter is too small, by means of a fine sterile prosthetic object designed for this purpose, to prevent the blood vessel from narrowing again during closure (Figure 9). In very rare cases, we can perform a bypass (Figure 10). The quality of the work is inspected directly as the arteriography procedure is being performed so as to make certain that there are no technical defects that could compromise the results of the operation.

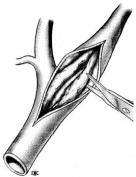

Figures 7

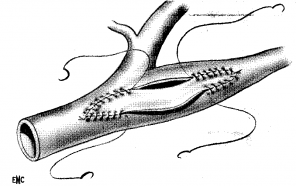

Figure 8 Figure 9 Figure 10
This operation may be recommended under local or general anaesthesia depending on the medical requirements of the patient and on his wishes. Local anaesthesia allows us optimal monitoring of the patient during the operation; however, we respect the wishes of patients who request total anaesthesia.
When using the endovascular route, the puncture is made in the fold of the groin or in rare cases the crook of the arm or the base of the neck, and using this route to navigate the blood vessels, a stent will then be fitted to reopen the stenosed carotid artery (Figures 11). This procedure is performed with a protective filter (Figures 12 – 13) temporarily placed beyond the work area, the purpose of which is to catch any debris that may migrate during the procedure and cause a stroke as a result. At the end of the procedure, the stent remains permanently in place and will be integrated into the blood vessel over time, while the filter is removed with any debris it contains. In the interest of precision, this procedure is most often performed under total anaesthesia, but can be done under local anaesthesia if necessity dictates.

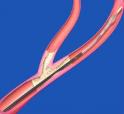


Figures 11

Figure 12
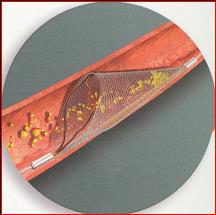
Figure 13
Post-operative period
After the operation, the patient is monitored for one night in intensive care to stabilise all of his parameters and therefore optimise the outcomes of the operation.
If there are no complications, the patient can return home without delay.
After the operation, the patient will be followed up over the long term by the representative who referred him to us; however, the patient can of course be followed up by us if he wishes and if he has no representative. In any event, the patient will not be left to his own devices.
