
General information and symptomatology
Arteries are natural conduits, like small pipes, that convey blood from the heart to the muscles and organs to feed them. The walls of these vessels can sometimes become diseased and dilated. Instead of maintaining a straight line, they become like pockets. These are called aneurysms. These aneurysms can be found wherever there are arteries, and thus throughout the human body.
There are however areas where they are more common: Distal abdominal aorta (Figure 1) > iliac art. > popliteal art > common femoral art. > aortic arch and descending thoracic aorta > carotid arteries > others.
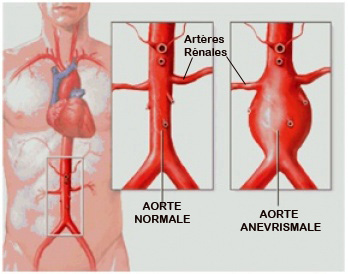

Figure 1 Figure 2
They are partly hereditary, are normally linked to atheromatous disease and are consequently linked to cardiovascular risk factors which themselves predispose to atheromatosis:
- Smoking
- Diabetes
- Cholesterol
- High blood pressure
- Hereditary determinants
- Significant metabolic disorders (haemodialysis, etc.)
Once aneurysms are present, their growth is clearly favoured by high blood pressure if it is poorly controlled.
Their presence does not always produce symptoms. They are sometimes painful or can manifest by compressing an adjacent organ: nerve, vein, visceral structure, vertebrae, etc. They can be felt on abdominal palpation (pulsatile mass). From a certain size, they can develop dangerously to the point of splitting, followed by total rupture (Figure 2): at this stage, any massive haemorrhaging in the abdomen or chest is often fatal. They are often filled with clots (coagulated blood) and can therefore become thrombotic (blocked) or embolic (release into the circulatory system small fragments that become lodged in the most distal arteries).
As you can see, this is a very serious disease that needs to be clearly understood in order to determine whether such threats are present or not.
Assessment
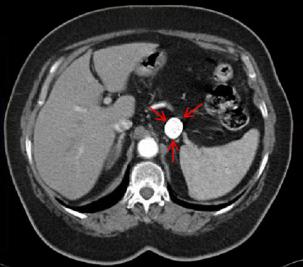
Whenever this problem is suspected, it is advisable to come in for a consultation. Diagnostic screening for this type of damage is performed by ultrasound (Figure 3) or CT scan. It will be more accurately documented by Angioscan (Figures 4), by arteriography (Figure 5) or, in cases of allergic reaction to the contrast agent, by nuclear magnetic resonance or MRI (Figure 6). In cases of renal insufficiency, we also have the option of performing CO2 arteriography which is harmless to the kidneys.
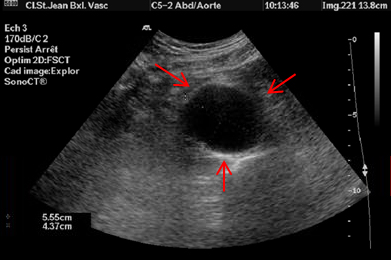
Figure 3
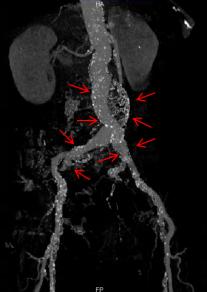
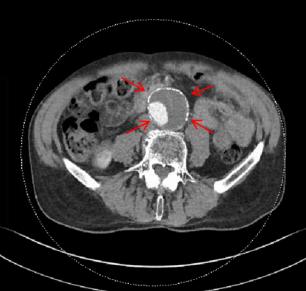
Figures 4
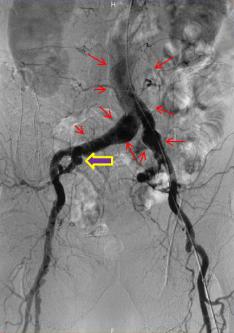

Figures 5
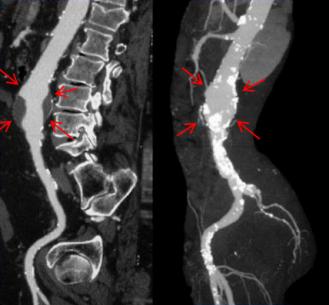
Figure 6
Treatment
After evaluating the problem and your overall state of health (blood test, cardiopulmonary examination) we will discuss the treatment options with you.
- Irrespective of the treatment considered, medical treatment is prescribed to stabilise all of the risk factors taken down in the general information.
- In some cases, there is no indication for surgery as the risk of rupture or complications is still very low. You will receive regular monitoring which will be clearly explained to you and blood pressure stabilisation will be vital. You will be prescribed anti-platelet medication.
- If necessary, surgical treatment is recommended. As far as possible, we give priority to treatment by endovascular route which is decidedly gentler on the body than treatment by open surgery.
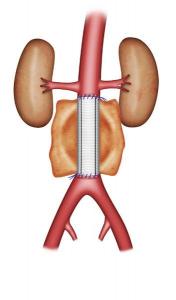
- Treatment by endovascular route has the advantage of being a scar-free treatment and generally is decidedly gentler on the body than conventional surgery. This is why it is the preferred form of intervention, wherever possible, if surgery is required; this is an important feature of our approach and all of the related state-of-the-art technologies are well managed and applied at Clinic Saint-Jean. They will no doubt be employed by the surgeon himself and he will follow your progress over the long term. The procedure involves inserting a metal-reinforced prosthesis. It is fully retracted in a thin sheath, inserted into the aorta, and then deployed. It consequently isolates the aneurysm from any circulation, thereby eliminating the risk of it developing to the point of rupture (Figure 7).
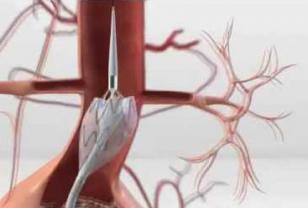

Figures 7
Here is an example of an aneurysm treated by us: the preoperative photos are the ones taken earlier on at “Assessment”, except for Figure 6 which relates to another case. This case is in itself somewhat special since the aneurysm encompasses both iliac arteries under the aorta and to the right; it descends to the iliac bifurcation, and this will necessitate preliminary exclusion of the right internal iliac artery by embolisation using small metal coils (Figure 8). If this embolisation is not performed, complete exclusion of the aneurysm will not be achieved and as it is still being infused, it remains under tension and at risk of rupture.
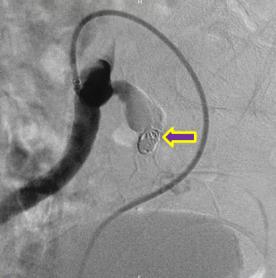
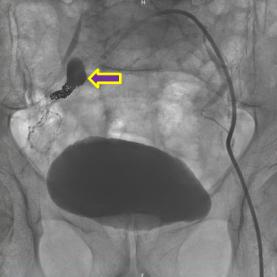
Figures 8
After the endoprosthesis has been fitted (Figure 9), the aneurysm is totally excluded from circulation. The risk of rupture or complication is removed. However, monitoring is still necessary.


Figures 9
Treatment by open surgery is an older and more rigorous technique than endovascular surgery as it requires laparotomy (substantial abdominal incision). It is nonetheless still indicated and has the advantage of being more reliable over the long term for aortic endoprostheses. It is recommended, among other reasons, when for technical reasons it is not possible to fit an aortic endoprosthesis. It involves removing the aneurysm and replacing it with a special synthetic prosthesis (Figure 10). Naturally, this procedure is performed at Clinic Saint-Jean.

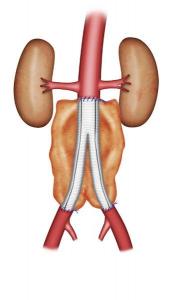
Figures 10
Treatment of other aneurysmal sites
Here is one of several examples of treatment of an aneurysm not located in the abdominal aorta, which was performed at our clinic. This is the case of a patient with an aneurysm in the splenic artery. This artery is located in the upper abdomen, extending towards the spleen (Figure 11).

Figures 11
Despite its circuitous route, it was possible to exclude this damaged area using coils (Figure 12).


Figures 12
Many other aneurysms have also been able to be treated using endovascular or conventional techniques or a hybrid of both types of techniques.
There will of course be subsequent follow-up by your surgeon.
